Recognizing Healthcare Worker Burnout and Ideas for Addressing It
This white paper explores key causes of burnout among healthcare workers. It shares findings from CareCredit's 2023 survey, including what employees value most and what may help clinics and hospitals better support and retain teams.
By Synchrony, Health & Wellness
Sep 26, 2025 - 8 min read

Burnout is a prevalent issue throughout the workforce, but especially in the healthcare sector.1 It has resulted in significant staffing shortages that must be addressed to maintain an adequate healthcare system.2 Recognizing that healthcare worker burnout affects systems everywhere is the first step toward facilitating a healthy workplace.
Fortunately, there are multiple potential answers to the question of how to prevent healthcare worker burnout. This white paper outlines key drivers of healthcare provider burnout and shares findings from the 2023 CareCredit Staff Burnout Survey on what staff value most. It also offers four practical strategies to reduce burnout and improve retention.
Burnout has long been a reason healthcare professionals leave the field. According to a 2025 National Council of State Boards of Nursing study, 39.9% of nurses surveyed plan to leave the profession within the next five years, and among them, 41.5% cited stress and burnout as the primary reason.3
The driving forces of burnout are numerous and may be attributed to different factors depending on employment motivations. These motivations have been shown to vary from one generation of employees to the next. Age diversity in healthcare professionals currently ranges from baby boomers to Generation Z.4 This diversity shapes various communication styles, tech adoption, work-life expectations and openness to feedback on healthcare teams.5 Therefore, the contributing factors to burnout and burnout solutions may vary from one group to the next.
While much attention has been given to the burnout experienced by physicians and nurses, other healthcare staff are also vulnerable to burnout. This can have a detrimental effect on the quality of patient care.6
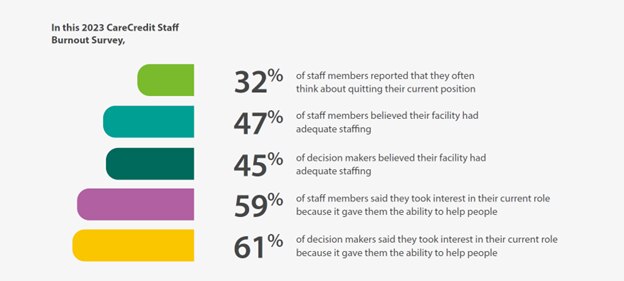
Burnout in healthcare is a public health concern. It’s essential to identify and relieve the factors contributing to staffing shortages and burnout in healthcare staff. To better understand the root causes, CareCredit surveyed 150 decision-makers and 200 staff members. The findings highlight actionable strategies to reduce burnout and improve retention.
Key Factors Fueling — and Easing — Burnout in Healthcare
The 2023 CareCredit Staff Burnout Survey uncovered shared stressors among healthcare staff and decision-makers, but also some key differences in motivation and job satisfaction.

When asked about the challenges that contributed to stress from their jobs, common trends emerged:
- Staffing shortages were primary contributors for both staff members and decision-makers.
- Both groups indicated that the burdensome documentation and regulatory issues limited their ability to spend time helping patients.
- This contributed to staff concerns that patient well-being was being compromised.
- Staff members felt they did not have sufficient time to help everyone or complete all their tasks.
There were also some indications that burnout factors affected staff members more than decision-makers:
- Approximately 68% of staff members reported they did not feel they had a fulfilling role, but this was much lower for decision-makers (35%).
- Up to 43% of staff members said they were at least somewhat likely to switch jobs in the next 12 months, versus only 29% of decision-makers.
- Meanwhile, up to 25% of staff members reported they would consider leaving the healthcare industry altogether.
These findings may explain why understaffing and inability to help all patients were contributors to job-related stress and suggest staffing shortages continue to affect healthcare facilities.
Additionally, some discrepancies in perceptions reported by decision-makers versus staff members merit further consideration and potential action. Decision-makers overestimated the job satisfaction of their staff, with 79% of them believing staff satisfaction was somewhat or very high, whereas only 60% of their staff reported they were very or extremely satisfied with their job.
This may be due to biased perceptions based on the decision-makers’ own job satisfaction, as 83% reported feeling very or extremely satisfied with their job. Only 26% of decision-makers felt undervalued, while nearly 47% of staff members felt the same.
While many staff members said they entered healthcare by chance, most decision-makers reported a clear intent to work in the field. Both groups cited helping others as a top motivator, though staff members placed more emphasis on job stability (57%) and flexible hours (38%) than decision-makers did.
How can we help reduce burnout for healthcare administrators?
The CareCredit Staff Burnout survey identifies factors contributing to burnout among healthcare staff and decision-makers, as well as their primary motivations for initially entering the field and what keeps them engaged. Key retention factors should include sufficient compensation, benefits, workplace stability, appreciation and reducing administrative burdens.
Compensation and Wellness Benefits
Staffing shortages drive much of today’s burnout, but hiring more staff isn’t the only solution, nor is it always possible. Survey findings show that 36% of healthcare staff ranked salary as the most important job factor. Yet only 42% were satisfied with their pay, compared to the 64% of decision-makers who were happy with their pay.
One straightforward way to help address burnout challenges across the industry is to prioritize wellness for healthcare staff.
Indeed, the second most valued element reported by staff members in the 2023 CareCredit Staff Burnout Survey was benefits, and those benefits all tied back to physical, financial and mental wellness, as well as the ability to take time off for family caretaking.
The largest portions of healthcare staff placed top priority on coverage for care related to:
- Medical
- Dental
- Vision
- Paid time off
- Paid sick leave
But most staff members (>50%) also valued:
- Life insurance
- Retirement planning
- Prescription and pharmacy benefits
- Family leave
- Disability benefits
- Mental health coverage
Provision of these benefits could potentially help the healthcare industry retain more employees.
Establish a Stable but Flexible Workplace Environment
While benefits ranked slightly higher, the workplace environment was nearly as important to healthcare staff. Of those surveyed in the 2023 CareCredit Staff Burnout Survey, many respondents cited job stability (57%) and flexible hours (38%) as key motivators. Organizational interventions such as workload reduction, decreasing time spent on documentation and allowing breaks without interruption are viewed by clinicians as ways to reduce burnout and improve well-being in healthcare workers.7
Though dedicated mental health resources are often recommended to reduce burnout, research and healthcare worker burnout statistics show that healthcare workers prefer interventions that better enable them to deliver care to patients.7
In the 2023 CareCredit Staff Burnout Survey, staff prioritized wellness benefits, such as paid time off, sick leave and medical coverage, suggesting a preference for managing their own well-being when supported.

Foster a Culture of Appreciation
The 2023 CareCredit Staff Burnout Survey showed that 47% of staff and 26% of decision-makers felt undervalued. A Grant Thornton survey found that healthcare workers receive feedback less than half as often as those in other fields, with 34% receiving it only once a year.1 Timely feedback may not only help address performance issues but also strengthen the employee-manager connection and reinforce staff value.

Relieve Administrative Burden
Beyond challenges in meeting patient needs, staff in the 2023 CareCredit Burnout Survey cited administrative tasks as a major source of frustration, often pulling focus from patient care. Reviewing workflows and addressing bottlenecks with the right programs and technology, such as third-party financing solutions, can lead to long-term time savings and improved efficiency.

Technological innovations may help but also hinder healthcare workers
Documentation burden remains a key contributor to clinician burnout, especially when electronic health record (EHR) systems are tied to reimbursement requirements.8 A survey of Canadian doctors at a mental health organization found that 26% of respondents met the criteria for burnout, with 61% of those attributing it to electronic health record (EHR) use. While over half believed EHRs improved communication and 75% felt more proficient using the system, only 38% agreed that EHRs supported high-quality care.9
Physicians participating in accountable care organizations (ACOs) may face higher documentation burdens than those in other value-based programs, partly because of potential overlapping billing and quality-reporting demands. Such extensive EHR use may leave less time for direct patient interaction and contribute to clinician burnout.
Efforts like the American Medical Informatics Association (AMIA) 25×5 initiative aim to reduce this documentation burden by 75% through better workflows, interoperability and system usability.10
Four strategic goals drive the AMIA’s 25x5 initiative:
- Wide adoption and utilization of task force tools and exemplars’ solutions by health professionals to reduce documentation burden across healthcare organizations in the United States10
- Greater funding for research and process improvements related to the mitigation of documentation burden10
- Increased identification of strategic initiatives to reduce the burden within U.S. healthcare organizations10
- Improved perception of documentation burden among health professionals10
Strategies to ease the documentation load on clinicians and other decision-makers may include minimizing unnecessary documentation, clarifying coding rules, expanding team documentation, delegating tasks, optimizing inbox routing and embracing digital tools and workflow improvements.
Practices that apply these approaches can potentially alleviate clerical burden, giving providers more time for patient care and may help reduce burnout.

The administrative burden is heavy
A Google Cloud and Harris Poll Survey found that clinicians spend at least 28 hours per week on administration tasks, while medical office staff spend an average of 34 hours weekly on admin. Payors’ claims staff spend 36 hours weekly on admin tasks, including 10.2 hours on documentation.11
Aligned with this, 30% of staff members from the 2023 CareCredit Staff Burnout Survey indicated they had responsibilities in billing.
At the same time, a May 2025 KFF poll reported that 36% of U.S. adults postponed or skipped needed medical care in the past year due to cost. Nearly two in ten adults overall (18%) said their health got worse as a result, with uninsured adults under age 65 about twice as likely as their insured peers to report worsening health (42% vs. 20%).12 These findings underscore how cost-related care avoidance may significantly harm patients’ health outcomes.
The 2023 CareCredit Staff Burnout Survey findings indicated that most healthcare staff and decision-makers took interest in their current role for the ability to help people, and patients’ negative experiences with billing practices may contribute to negative sentiments by healthcare employees, as well. According to a recent Flywire survey, 80% of patients report wanting to pay medical bills in installments, and 60% can’t afford to cover unexpected care costs in a single payment.13
With trends toward value-based care continuing, patients’ perceptions — and willingness to return to a practice — are an important business driver for providers.

CareCredit offers flexible financing options with the CareCredit credit card to help patients manage out-of-pocket health and wellness expenses at over 285,000 enrolled locations across the U.S. CareCredit helps providers minimize accounts receivable and reduce the administrative burden associated with billing by helping streamline the medical billing process.
Take Control to Prevent Healthcare Worker Burnout
Burnout and staffing shortages exacerbated by the pandemic form a vicious cycle — contributing to healthcare workers feeling unable to provide adequate patient care, and often resulting in moral distress, safety concerns and further workforce depletion.14
The 2023 CareCredit Staff Burnout Survey revealed that burnout remains a pervasive issue among healthcare workers. It appears that many decision-makers overestimate the satisfaction of their staff employees. With as many as 43% of staff members reporting that they are somewhat likely to leave their current role, staffing shortages that contribute to the feeling of burnout may increase in the near future.
Numerous strategies may be implemented to retain healthcare staff, from prioritizing benefits and policies that encourage employee welfare and feelings of appreciation to relieving their administrative burden through streamlined documentation processes and innovative technologies, as well as outsourced tasks — like billing — that can be performed by someone outside of the healthcare institution.
Offering the CareCredit healthcare credit card as a patient payment option may help relieve healthcare worker burnout by reducing administrative burden. Ultimately, better job satisfaction can result from prioritizing healthcare staff wellness and feelings of appreciation, in addition to reducing the number of hours spent on administrative tasks. In turn, enhancing the quality of experience for healthcare staff may enhance the quality of care for the patients.
Offer Flexible Financing at Your Practice
If you are looking for a way to connect your patients or clients with flexible financing that empowers them to pay for the care they want and need, consider offering the CareCredit credit card as a financing solution. CareCredit allows cardholders to pay for out-of-pocket health and wellness expenses over time while helping enhance the payments process for your practice or business.
When you accept CareCredit, patients or clients can see if they prequalify with no impact to their credit score, and those who apply, if approved, can take advantage of special financing on qualifying purchases.* Additionally, you will be paid directly within two business days.
Learn more about the CareCredit credit card as a financing solution or start the provider enrollment process by filling out this form.
Healthcare payment and financing solution
The CareCredit health and wellness credit card helps improve the payment experience for patients and clients, and your financial performance.
Get Started
*Subject to credit approval.
The information, opinions and recommendations expressed in the article are for informational purposes only. Information has been obtained from sources generally believed to be reliable. However, because of the possibility of human or mechanical error by our sources, or any other, Synchrony and any of its affiliates, including CareCredit, (collectively, “Synchrony”) does not provide any warranty as to the accuracy, adequacy or completeness of any information for its intended purpose or any results obtained from the use of such information. All statements and opinions in this article have been evaluated and are supported by the expert reviewer. The data presented in the article was current as of the time of writing. Please consult with your individual advisors with respect to any information presented.
© 2025 Synchrony Bank.
Sources:
1 “Staffing and well-being factors afflict healthcare workers,” Grant Thornton. June 15, 2023. Retrieved from: https://www.grantthornton.com/insights/articles/health-care/2023/staffing-and-well-being-factors-afflict-healthcare-workers
2 “Health Worker Burnout,” U.S. Department of Health and Human Services. Accessed September 11, 2025. Retrieved from: https://www.hhs.gov/surgeongeneral/reports-and-publications/health-worker-burnout/index.html
3 “NCSBN research highlights small steps toward nursing workforce recovery; burnout and staffing challenges persist,” NCSBN. April 17, 2025. Retrieved from: https://www.ncsbn.org/news/ncsbn-research-highlights-small-steps-toward-nursing-workforce-recovery-burnout-and-staffing-challenges-persist
4 Tan, J. X., et al. “Generational effect on nurses’ work values, engagement and satisfaction in an acute hospital,” Journal of Nursing Management. 2023. Retrieved from: https://pmc.ncbi.nlm.nih.gov/articles/PMC10061355/
5 Sanches, R. S., et al. “Generational diversity in nursing practice environments: Scoping review,” BMC Nursing. December 19, 2024. Retrieved from: https://bmcnurs.biomedcentral.com/articles/10.1186/s12912-024-02607-3
6 Cohen, Catherine et al. “Workplace intervention to improve well-being and reduce burnout for nurses, physicians and allied healthcare professionals: A systematic review,” BMJ Open. June 29, 2023. Retrieved from: https://bmjopen.bmj.com/content/bmjopen/13/6/e071203.full.pdf
7 Aiken, Linda H. et al. “Physician and nurse well-being and preferred interventions to address burnout in hospital practice,” July 7, 2023. JAMA Health Forum. Retrieved from: https://jamanetwork.com/journals/jama-health-forum/fullarticle/2807049
8 Levy, Deborah R. et al. “Reflections on the documentation burden reduction AMIA plenary session through the lens of 25 × 5,” Applied Clinical Informatics. January 4, 2023. Retrieved from: https://pmc.ncbi.nlm.nih.gov/articles/PMC9812582/
9 Tajirian, T., et al. “Five years of physician engagement in a Canadian mental health organization: Assessing the impact on EHR burden through a mixed methods study,” August 2024. Retrieved from: https://www.researchgate.net/publication/390281091_Five_Years_of_Physician_Engagement_in_a_Canadian_Mental_Health_Organization_Assessing_the_Impact_on_EHR_Burden_through_a_Mixed_Methods_Study_Preprint
10 “AMIA 25x5: Reducing documentation burden to 25% of current state in five years,” Accessed September 11, 2025. Retrieved from: https://amia.org/about-amia/amia-25x5
11 “Measuring the administrative burden on U.S. healthcare workers — and how generative AI can help,” 2024. Retrieved from: https://services.google.com/fh/files/misc/measuring_admin_burden_2024_ebook.pdf
12 Sparks, Grace et al. “Americans’ challenges with healthcare costs,” KFF. July 11, 2025. Retrieved from: https://www.kff.org/health-costs/issue-brief/americans-challenges-with-health-care-costs/
13 “Flywire survey uncovers increasing demand for flexible, patient-centric payment solutions in U.S. healthcare,” Flywire. October 29, 2024. Retrieved from: https://www.flywire.com/news/flywire-survey-uncovers-increasing-demand-for-flexible-patient-centric-payment-solutions-in-u-s-healthcare
14 Linzer, Mark et al. “Burnout in modern-day health care: Where are we, and how can we markedly reduce it? A meta-narrative review from the EUREKA project,” Health Care Management Review. April-June 2025. Retrieved from: https://journals.lww.com/hcmrjournal/fulltext/2025/04000/burnout_in_modern_day_health_care__where_are_we,.2.aspx

