Recognizing Burnout in Healthcare Staff and Ideas for Addressing It
The contributing factors to healthcare worker burnout and the results of a valuable survey that assesses the factors of employment that healthcare workers most value.
By Synchrony, Health & Wellness
Posted Apr 18, 2024 - 15 min read

Burnout is a prevalent issue throughout the workforce, but especially in the healthcare sector,1 and it has resulted in significant staffing shortages that must be addressed to maintain an adequate healthcare system.2
Fortunately, there are multiple potential solutions to this prevalent issue. In this white paper, we will review the contributing factors to healthcare worker burnout and the results of a valuable survey that assesses the factors of employment that healthcare workers most value. We will then use those results to present four best practices for reducing burnout and retaining employees.

“The Great Resignation,”
a mass exodus of employees from their positions, was triggered by the Coronavirus pandemic, and attributed to sentiments of inadequate compensation, limited advancement opportunities and general feelings of being disrespected in the workplace.3 Alongside the Great Resignation, another troubling trend has emerged: burnout among healthcare workers.
Burnout has been demonstrated in numerous national surveys
and cited as the primary reason for healthcare workers leaving the field.4 This was an issue even before Coronavirus pandemic, but the pandemic only worsened it.5 In 2022, 40% of doctors and 49% of nurses reported they were experiencing burnout, and 32% of nurses were planning to leave their profession within the next year.6 Burnout is cyclical, too, resulting in staffing shortages and increases in the workloads of remaining workers, contributing to further burnout.7,8 In fact, healthcare workforce burnout has become such a serious issue that, in 2019, the World Health Organization (WHO) added it to the International Classification of Diseases as an “occupational phenomenon” (but not as a medical condition).9
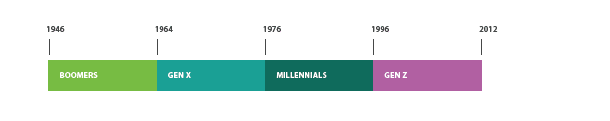
The driving forces of burnout are numerous
and may be attributed to different factors depending on employment motivations, and these motivations have been shown to vary from one generation of employees to the next. For perhaps the first time, there are four generations currently in the workforce: Baby Boomers (born 1945-1960), Generation X (born 1960-1980), Millennials (or Generation Y; born 1980-2000) and Generation Z (born after 2000). Each generation approaches their work with a different perspective and different values, as well as how they view job satisfaction.10 Thus the contributing factors to burnout and methods of addressing them may vary from one group to the next.
Previously, many articles have focused on the burnout of physicians and nurses,11–15
but healthcare staff play an unquestionable supportive role in healthcare16 and are not immune to burnout themselves.17 This strains everyone in the healthcare industry, from the workers at the front desk18 or radiologists in the lab,19 to the nurses and physicians providing patient-facing care,20 and negatively impacts patient care.21 Patients have experienced delayed appointments and surgeries due to these shortages, and have had less access to healthcare facilities due to shortened hours.22

As a matter of public health,
it is essential to identify and relieve the factors contributing to burnout in healthcare staff. To help the industry better understand the root causes of burnout and staffing shortages, CareCredit recently performed a survey of 150 decision makers and 200 staff members in healthcare to assess ongoing sentiments of burnout and contributing factors. The results of this survey provide guidance on potential approaches to reduce burnout and retain employees in healthcare.

Key Contributing Factors Driving — and Combatting — Burnout
Results from the 2023 CareCredit Staff Burnout survey indicated there were some common stressors between healthcare staff and decision makers, but also some differences between these two groups regarding motivating factors and job satisfaction that are worth noting.

When asked about the challenges that contributed to stress from their jobs, common trends emerged:
- Staffing shortages were primary contributors in both staff members and decision makers.
- Both groups indicated the burdensome documentation and regulatory issues limited their ability to spend time helping patients:
- This led to staff members’ feelings that patients’ well-being was being compromised.
- Staff members felt they did not have sufficient time to help everyone or complete all their tasks.
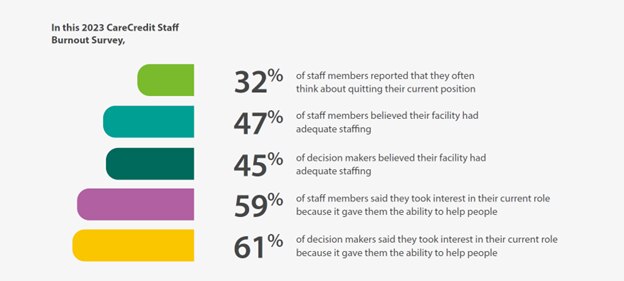
In this 2023 CareCredit Staff Burnout Survey,
- 32% of staff members reported that they often think about quitting their current position
- 47% of staff members believed their facility had adequate staffing
- 45% of decision makers believed their facility had adequate staffing
- 59% of staff members said they took interest in their current role because it gave them the ability to help people
- 61% of decision makers said they took interest in their current role because it gave them the ability to help people
There were also some indications that burnout factors affected staff members more than decision makers:
- Approximately 68% of staff members reported they did not feel they had a fulfilling role, but this was much lower for decision makers (35%).
- Up to 43% of staff members said they were at least somewhat likely to switch jobs in the next 12 months, versus only 29% of decision makers.
- Meanwhile, up to 25% of the staff members reported they would consider leaving the healthcare industry altogether.
These findings may explain why under-staffing and inability to help all patients was such a contributor to job-related stress, and suggest staffing shortages continue to affect healthcare facilities.
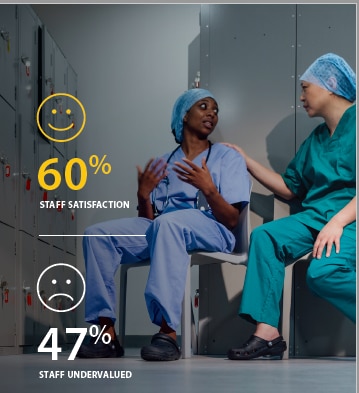
Additionally, some discrepancies in perceptions reported by decision makers versus staff members merit further consideration and potential action. Decision makers overestimated the job satisfaction of their staff, with 79% of them believing staff satisfaction was somewhat or very high, whereas only 60% of their staff reported that they were very or extremely satisfied with their job. This may be due to biased perceptions based on the decision makers’ own job satisfaction, as 83% of them reported feeling very or extremely satisfied with their job. In addition, only 26% of decision makers felt undervalued, while nearly twice as many (47%) of staff members expressed that sentiment.
When examining the motivations of these two groups in healthcare, it was interesting to note that one of the most common responses for why staff members entered healthcare jobs was that they just fell into it — with no specific interest.
In contrast,
the most common response from decision makers was that they specifically wanted to work in healthcare. Both groups were strongly motivated by helping others — it was one of the top three responses when asked what contributed to their interest in their current role. Other top factors that staff members cited as the reasons for initial interest in their current role were job stability (57%) and flexible working hours (38%); these were both noticeably higher priorities for staff members than for decision makers.
How can we help reduce burnout for healthcare administrators?
With guidance from the CareCredit Staff Burnout survey that indicates the factors contributing to burnout of healthcare staff and decision makers, as well as their primary motivations for entering the job in the first place, it becomes clear that there are key factors that can contribute to retaining both groups in the healthcare industry. These factors primarily include focus on providing sufficient compensation, benefits, workplace stability and appreciation, as well as reducing the administrative burdens of the job.
Compensation and Wellness Benefits
With so much burnout manifesting as a product of staffing shortages, one obvious solution to reducing burnout is, of course, to hire more staff. Up to 36% of healthcare staff from the 2023 CareCredit Staff Burnout Survey indicated salary was the most important element of their job, yet only 42% of them were satisfied with their current level of compensation, versus 64% of decision makers.
Some experts have indicated that a 10%-20% increase in salary is needed in healthcare to adjust for inflation.23
However, given budgetary limitations, salary increases are not always feasible to retain existing staff members or recruit new ones. Other factors, including wellness benefits, can have substantial influence on employment.

One straightforward way to help address burnout challenges across the industry is to prioritize wellness amongst healthcare staff.
In a 2020 report from Medscape that surveyed healthcare workers across generations, approximately 48% of Generation X physicians, 39% of Baby Boomers and 38% of Millennials reported experiencing burnout.24 Carol A. Bernstein, MD, Professor and Vice Chair for Faculty Development and Wellbeing in the Departments of Psychiatry and Behavioral Science and Obstetrics and Gynecology and Women's Health at Montefiore Medical Center and the Albert Einstein College of Medicine, posited that the higher levels of burnout among Generation X physicians could be a result of them being mid-career. This is a time where burnout is typically the highest, as well as their need to juggle multiple roles outside of the workplace, including caring for children as well as elderly parents.25 Indeed, the second most valued element reported by staff members in the 2023 CareCredit Staff Burnout Survey was benefits, and those benefits all tied back to physical, financial and mental wellness, as well as the ability to take time off for family caretaking.
The largest portions of healthcare staff placed top priority on coverage for care related to:
- Medical
- Dental
- Vision
- Paid time off
- Paid sick leave
But most staff members (>50%) also valued:
- Life insurance
- Retirement planning
- Prescription and pharmacy benefits
- Family leave
- Disability benefits
- Mental health coverage
Provision of these benefits could potentially help the healthcare industry retain more employees.

Establish a Stable but Flexible Workplace Environment
Though benefits were prioritized slightly more, workplace environment was almost equally valued by healthcare staff.
In addition to the goal of helping others, most staff members (57%) were motivated to enter their current position because of job stability, and 38% also placed high value on flexible working hours. Ensuring a consistent role and providing flexible scheduling has actually been shown to improve staff performance and mental health, as it ensures they have sufficient time to cope with job stress and other challenges.23
It should be noted that provision of dedicated mental health resources is often mentioned as a potential intervention to help manage healthcare worker stress and burnout,2,26,27 but a study showed that people who work in healthcare prefer interventions that help them to better manage how they deliver care to patients.28 In the 2023 CareCredit Staff Burnout Survey, staff members prioritized wellness-related benefits such as paid time off and paid sick leave, as well as medical coverage, suggesting that they manage their own wellness, given the opportunity to do so. Aligned with that concept, experts have stated that stigma surrounding care for mental health is often the greatest impediment to seeking care, and this can be overcome through normalization of discussions about mental health in the workplace and an understanding and appreciation for seeking help.29

Foster a Culture of Appreciation
According to a report in Vatornews, 69% of clinicians who admitted to feeling burned out reported they did not feel valued.5 Strategies that aim to address this could help establish a productive, engaged workforce that helps healthcare organizations reduce costs, improve patient outcomes and stay competitive. In the 2023 CareCredit Staff Burnout Survey, 47% of staff reported feeling undervalued, as did 26% of decision makers.
A previous report suggested that more timely feedback on performance could be a way to address employees’ sense of feeling undervalued.1 A survey by Grant Thornton revealed that little more than half as many people who work in healthcare receive feedback at least weekly compared to people who work in other professions. In fact, 34% of healthcare workers only received feedback on an annual basis.1 Regular feedback on performance, the survey suggests, is not only beneficial for addressing issues, but also establishes a connection between employees and their managers that clearly demonstrates the employees’ value.1

Relieve Administrative Burden
In addition to inability to help all of the patients, respondents to the 2023 CareCredit Staff Burnout Survey also reported frustrations with administrative tasks as one of their least favorite parts of the job, as these were the very factors that took time away from patient care. Various methods are being utilized to reduce administrative burden, from streamlining documentation practices30 to technological assistance such as digital intake and check-in methods.31 Investing a little time up front to analyze workflow processes, identify bottlenecks, and utilizing technologies that can address those bottlenecks can save many hours in the long run.

It is important to note that technological innovations may affect various generations of employees differently.
In the generational survey by Medscape, Baby Boomers cited the introduction of new technology as a top stressor, and the increasing use of electronic health records (EHRs) as a top three factor for burnout, whereas younger generations ranked this as one of the lowest contributing stressors to their work.24 Research has found that some technologies like automatic check-ins easily reduce administrative burden for healthcare staff, whereas others like EHRs have increased that burden by introducing duplicative records-keeping practices.32 This was often due to insufficient accessibility or poor integration of multiple softwares. One study found that in addition to spending up to two hours each night doing administrative work, physicians spend nearly two hours on EHRs and desk work during the day for every one hour spent with patients.33 Thus, the introduction of technologies designed to reduce administrative burden can contribute to further stress if not streamlined properly. The American Medical Informatics Association’s 25x5 initiative aims to reduce documentation burden by 75% by 2025.34
The AMIA’s 25x5 initiative is driven by four strategic goals:
- Wide adoption and utilization of task force tools and exemplars’ solutions by health professionals to reduce documentation burden across U.S. healthcare organizations.
- Greater funding for research and process improvements related to mitigation of documentation burden.
- Increased identification of strategic initiatives to reduce burden within U.S. healthcare organizations.
- Improved perception of documentation burden among health professionals.

Efforts to review internal processes to help reduce duplicative, inefficient work can also reduce the administrative burden. Hawaii Pacific Health’s “Getting Rid of Stupid Stuff” program, for example, has saved 1,700 nursing hours per month across the health system.35

Another tremendous contributor to administrative burden is the process of billing.
Due to its complexity, it is estimated that about 1/4 of the healthcare labor force is involved in billing and related administrative tasks, which require 7.7 times as many full-time workers compared to billing in other industries.36

Aligned with this, 30% of staff members from the 2023 CareCredit Staff Burnout Survey indicated they had responsibilities in billing. Research has estimated that administrators for a single office can spend as many as 36 hours per week dealing with billing-related matters, and it takes as many as seven administrators per 10 physicians just to handle billing activities.37
As many as one-third of patients from a previous study indicated that out-of-pocket costs and deductibles were too high for them to afford.38 This contributes to substantial stress for the patients and negative perceptions of healthcare — up to 22% of patients who received an unexpected bill from their provider said they would never want to go to that doctor again – which is critical, as patient experience is an important part of provider selection.39 The 2023 CareCredit Staff Burnout Survey findings indicated most healthcare staff and decision makers took interest in their current role for the ability to help people — and patients’ negative experiences with billing practices may contribute to negative sentiments by the healthcare employees, as well. Most patients express interest in flexible payment options,38 and many utilize payment plans offered by hospitals, when offered.40 With trends towards value-based care continuing, patient’s perceptions — and willingness to return to a practice — is an important business driver for providers.

CareCredit, a Synchrony Solution,
offers flexible financing options with the CareCredit credit card to help patients manage out-of-pocket health and wellness expense at over 266,000 enrolled locations across the US. CareCredit helps providers minimize accounts receivable and reduce administrative burden associated with billing.
Concluding Thoughts
Burnout and staffing shortages exacerbated by the pandemic form a vicious cycle, ultimately depleting the healthcare workforce, which can compromise patient care. The 2023 CareCredit Staff Burnout Survey revealed that burnout remains a pervasive issue among healthcare workers, it appears that many decision makers overestimate the satisfaction of their staff employees. With as many as 43% of staff members reporting that they are somewhat likely to leave their current role, staffing shortages that contribute to the feeling of burnout may increase in the near future.
Numerous strategies may be implemented to retain healthcare staff, from prioritizing benefits and policies that encourage employee welfare and feelings of appreciation to relieving their administrative burden through streamlined documentation processes and innovative technologies, as well as outsourced tasks that can be performed by someone outside of the healthcare institution — like billing.

Offering the CareCredit healthcare credit card as a patient payment option may help relieve healthcare worker burnout, by reducing administrative burden. Ultimately, better job satisfaction can result from prioritizing healthcare staff wellness and feelings of appreciation, in addition to reducing the number of hours spent on administrative tasks. In turn, enhancing the quality of experience for healthcare staff can enhance the quality of care for the patients.
Download the full article to learn best practices for reducing burnout and retaining employees (PDF).
Healthcare payment and financing solution
The CareCredit health and wellness credit card helps improve the payment experience for patients and clients, and your financial performance.
Get Started* Subject to the representations and warranties in the Agreement with Synchrony.
This content is subject to change without notice and offered for informational use only. You are urged to consult with your individual advisors [and/or medical providers] with respect to any information presented. Synchrony and any of its affiliates, including CareCredit, (collectively, “Synchrony”) makes no representations or warranties regarding this content and accepts no liability for any loss or harm arising from the use of the information provided. Your receipt of this material constitutes your acceptance of these terms and conditions.
1 Grant Thornton. Staffing and well-being factors afflict healthcare workers. Grant Thornton. Published June 15, 2023. Accessed October 24, 2023. https://www.grantthornton.com/insights/articles/health-care/2023/staffing-and-well-being-factors-afflict-healthcare-workers
2 Centers for Disease Control and Prevention. Health Worker Burnout — Current Priorities of the U.S. Surgeon General. Accessed October 23, 2023. https://www.hhs.gov/surgeongeneral/priorities/health-worker-burnout/index.html
3 Parker K, Horowitz JM. Majority of workers who quit a job in 2021 cite low pay, no opportunities for advancement, feeling disrespected. Pew Research Center. Accessed October 23, 2023. https://www.pewresearch.org/short-reads/2022/03/09/majority-of-workers-who-quit-a-job-in-2021-cite-low-pay-no-opportunities-for-advancement-feeling-disrespected/
4 Ney E. A Treatment for America’s Healthcare Worker Burnout. Bain. Published October 11, 2022. Accessed October 12, 2023. https://www.bain.com/insights/a-treatment-for-americas-healthcare-worker-burnout/
5 Awan O. Healthcare Worker Burnout Is Rampant- Here’s What Should Be Done. Forbes. Accessed October 12, 2023. https://www.forbes.com/sites/omerawan/2023/03/08/healthcare-worker-burnout-is-rampantheres-what-should-be-done/
6 A Public Health Crisis: Staffing Shortages in Health Care | USC MPH. Online Masters in Public Health. Published October 25, 2022. Accessed June 6, 2023. https://mphdegree.usc.edu/blog/staffing-shortages-in-health-care/
7 Levins H. How Inadequate Hospital Staffing Continues to Burn Out Nurses and Threaten Patients. Penn LDI. Published January 9, 2023. Accessed October 12, 2023. https://ldi.upenn.edu/our-work/research-updates/how-inadequate-hospital-staffing-continues-to-burn-out-nurses-and-threaten-patients/
8 A Public Health Crisis: Staffing Shortages in Health Care | USC MPH. Accessed October 12, 2023. https://mphdegree.usc.edu/blog/staffing-shortages-in-health-care/
9 Burn-out an “occupational phenomenon”: International Classification of Diseases. World Health Organization. Published May 28, 2019. Accessed October 27, 2023. https://psychiatry.duke.edu/news/large-survey-identifies-toll-pandemic-health-care-worker-exhaustion
12 Alkhamees AA, Aljohani MS, Kalani S, et al. Physician’s Burnout during the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health. 2023;20(5):4598. doi:10.3390/ijerph20054598
13 California Medical Association. Study finds COVID-19 pandemic has driven physician burnout to an all time high. California Medical Association. Published September 20, 2022. Accessed October 24, 2023. https://www.cmadocs.org/newsroom/news/view/ArticleId/49885/Study-finds-COVID-19-pandemic-has-driven-physician-burnout-to-an-all-time-high
14 Gambaro E, Gramaglia C, Marangon D, Probo M, Rudoni M, Zeppegno P. Health Workers’ Burnout and COVID-19 Pandemic: 1-Year after—Results from a Repeated Cross-Sectional Survey. Int J Environ Res Public Health. 2023;20(12):6087. doi:10.3390/ijerph20126087
15 Melnikow J, Padovani A, Miller M. Frontline physician burnout during the COVID-19 pandemic: national survey findings. BMC Health Services Research. 2022;22(1):365. doi:10.1186/s12913-022-07728-6
16 Castro V. 4 strategies to reduce your practice´s administrative burden. Health Prime. Published September 23, 2021. Accessed October 24, 2023. https://www.hpiinc.com/educational-blog/4-strategies-to-reduce-your-practices-administrative-burden/
17 BWH Communications. COVID burnout hitting all levels of healthcare workforce. Harvard Gazette. Published March 31, 2023. Accessed October 24, 2023. https://news.harvard.edu/gazette/story/2023/03/covid-burnout-hitting-all-levels-of-health-care-workforce/
18 admin. Healthcare Providers Face Staffing Shortages in Front Desk Registration. PatientWorks. Published December 7, 2019. Accessed October 23, 2023. https://www.patientworks.com/healthcare-providers-face-staffing-shortages-in-front-desk-registration/
19 Murphy H. Radiologists once again rank among the most burned-out specialists. HealthImaging. Published February 2, 2023. Accessed October 23, 2023. https://healthimaging.com/topics/healthcare-management/medical-practice-management/radiologists-rank-among-most-burned-out
20 Thompson D. Almost Two-Thirds of U.S. Doctors, Nurses Feel Burnt Out at Work: Poll. US News & World Report. Published February 23, 2023. Accessed October 23, 2023. https://www.msms.org/About-MSMS/News-Media/healthcare-staffing-shortages-decrease-practice-risks
22 Neyra R. Medical Staffing Shortages Continue Into 2023. Billed Right. Published August 15, 2022. Accessed October 23, 2023. https://billedright.com/medical-staffing-shortages-continue/
23 Glatter R, Papadakos P, Shah Y. American Health Care Faces a Staffing Crisis. Time. Published online June 30, 2023. Accessed October 23, 2023. https://time.com/6291392/american-health-care-staffing-crisis/
24 Kane L. Medscape National Physician Burnout & Suicide Report 2020: The Generational Divide. Medscape. Published January 15, 2020. Accessed October 27, 2023. https://www.medscape.com/slideshow/2020-lifestyle-burnout-6012460
25 Delmonico K. Physician Burnout Rate Is Highest Among Generation X Doctors. Orthopedics This Week. Published March 26, 2020. Accessed October 27, 2023. https://ryortho.com/breaking/physician-burnout-rate-is-highest-among-generation-x-doctors/
26 Mental Health America. The Mental Health of Healthcare Workers in COVID-19. Mental Health America. Accessed October 23, 2023. https://mhanational.org/mental-health-healthcare-workers-covid-19
27 American Medical Association (AMA). Half of health workers report burnout amid COVID-19. American Medical Association. Published July 20, 2021. Accessed October 23, 2023. https://www.ama-assn.org/practice-management/physician-health/half-health-workers-report-burnout-amid-covid-19
28 Aiken LH, Lasater KB, Sloane DM, et al. Physician and Nurse Well-Being and Preferred Interventions to Address Burnout in Hospital Practice. JAMA Health Forum. 2023;4(7):e231809. doi:10.1001/jamahealthforum.2023.1809
29 Hamadeh R. Health workers’ mental health: Addressing the invisible global pandemic. STAT. Published November 10, 2022. Accessed October 24, 2023. https://www.statnews.com/2022/11/10/health-workers-mental-health-addressing-invisible-global-pandemic/
30 FPM Editors. 10 ways to reduce your administrative and documentation burden. Quick Tips: A Blgo from FPM Journal. Published August 15, 2022. Accessed October 23, 2023. http://localhost:4503/content/brand/aafp/pubs/fpm/blogs/inpractice/entry/reduce-administrative-burden.html
31 Landau J. The Challenges of Reducing Clinicians’ Administrative Burdens. Healthcare IT Today. Published June 3, 2022. Accessed October 24, 2023. https://www.healthcareittoday.com/2022/06/03/the-challenges-of-reducing-clinicians-administrative-burdens/
32 Howard J, Clark EC, Friedman A, et al. Electronic Health Record Impact on Work Burden in Small, Unaffiliated, Community-Based Primary Care Practices. J Gen Intern Med. 2013;28(1):107-113. doi:10.1007/s11606-012-2192-4
33 Sinsky C, Colligan L, Li L, et al. Allocation of Physician Time in Ambulatory Practice: A Time and Motion Study in 4 Specialties. Ann Intern Med. 2016;165(11):753-760. doi:10.7326/M16-0961
34 Report from the 25 By 5: Symposium Series to Reduce Documentation Burden on U.S.Clinicians by 75% by 2025. Published online August 6, 2021. Accessed October 30, 2023. https://www.dbmi.columbia.edu/wp-content/uploads/2021/08/25x5_Executive_Summary_V2.pdf
35 Ashton M. Getting Rid of Stupid Stuff. N Engl J Med. 2018;379(19):1789-1791. doi:10.1056/NEJMp1809698
36 Gottlieb JD, Shepard M. How Large a Burden are Administrative Costs in U.S. Health Care? | Econofact. Published online September 6, 2018. Accessed October 11, 2023. https://econofact.org/how-large-a-burden-are-administrative-costs-in-health-care
37 Frakt A. The Astonishingly High Administrative Costs of U.S. Health Care. The New York Times. https://www.nytimes.com/2018/07/16/upshot/costs-health-care-us.html. Published July 16, 2018. Accessed October 11, 2023.
38 Lagasse J. Paying for healthcare creates mental and financial health concerns. Healthcare Finance News. Published June 8, 2023. Accessed October 11, 2023. https://www.healthcarefinancenews.com/news/paying-healthcare-creates-mental-and-financial-health-concerns
39 Shryock T. Health care costs increasing physical and mental problems for patients. MedicalEconomics. Published June 7, 2023. Accessed October 11, 2023. https://www.medicaleconomics.com/view/health-care-costs-increasing-physical-and-mental-problems-for-patients
40 Survey: Patients prefer payment plans for healthcare costs. Flywire. Accessed October 11, 2023. https://www.flywire.com/resources/survey-patients-prefer-payment-plans-as-payment-option